
Throughout life, everyone is at some point susceptible to a severe spine injury. Whether your injury results from excessive lifting, a sedentary lifestyle, or a sports-related accident, spine injuries can result in a great deal of pain. Unfortunately, spine injuries can create serious limitations on your lifestyle. Recently, orthopedic surgeons have shifted their attention toward a new technique, known as minimally invasive spine surgery. Read on to learn more about minimally invasive spine surgery, and conditions it treats.
Minimally Invasive vs Open Spine Surgery
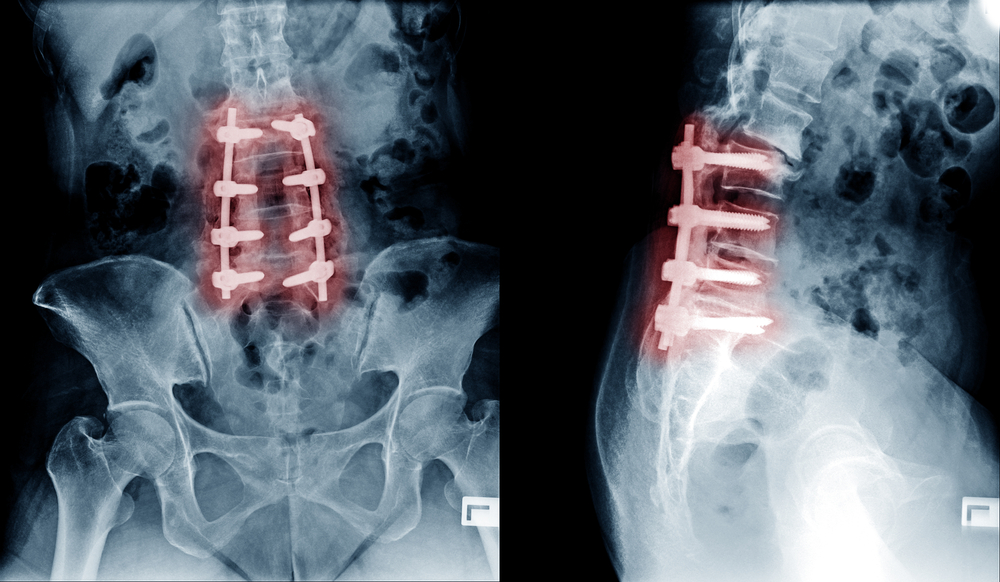
- Open Surgery: In standard open spine surgeries, orthopedic surgeons generally make a large incision– approximately 5-6 inches. This incision allows them to move the spinal muscles off to the side, granting them a full view of the spine. Then, the orthopedic surgeon can remove any damaged bones or disks. The operating surgeon can also stabilize the position of the spine by placing screws, cages, or even bone grafts to hasten the healing process.
- Minimally Invasive Surgery: Rather than cutting 6 inches of the skin surrounding the spine, orthopedic surgeons conducting minimally invasive surgery utilize a tubular retractor to gain access to the area that requires treatment. This grants surgeons the ability to see the damaged bone using fluoroscopy, an x-ray view that displays in real time. This heightened imaging also prevents a great deal of trauma. The tube, which remains inserted throughout the entire process, is also used to connect any surgical hardware to the spine. For the minimally invasive technique to be effective, the surgeon must locate the exact source of the pain. At the conclusion of the surgery, the retractor is removed, causing the muscles to return to their previous positions.
Why Orthopedic Surgeons Prefer Minimally Invasive Surgery
Despite a potentially repaired spinal structure, an open surgery could lead to several severe complications. Open spine surgery also grants the orthopedic surgeon far more access to the muscles and bones than they realistically need. Thus, open surgery creates a greater potential for problems to occur. Because of the decreased surgical zone, there is less bleeding, and also potential for an easier recovery.

When Is Minimally Invasive Spine Surgery Effective?
Spinal injuries rarely have the same effect on people. In fact, the pre existing condition of one’s spine can largely inform how their body reacts to particular injuries. Because of this, there is no clear, distinct solution to all spinal injuries. Some injuries require a greater degree of attention from orthopedic surgeons than others. Therefore, they cannot be easily treated with a minimally invasive approach. These are some of the most common injuries that are treatable using a minimally invasive approach.
5 Conditions Treated With Minimally Invasive Surgery
-
- Degenerative Disc Disease- Over time, the discs in the lumbar system naturally deteriorate. This process is inevitable, and is hastened by overuse of the spine, smoking, and sometimes genetics. The term “disease” is somewhat inaccurate, as discs degenerate regardless of external factors. After pinpointing the particular disk that is causing issues, the orthopedic surgeon will remove the disk.
- Herniated Discs- Lumbar discs are filled with a jelly-like substance that holds everything in place. When this substance is pushed outside of the normal area, this is called a herniated (or “slipped”) disc. Herniated discs are a common injury for people who frequently lift, whether occupationally or recreationally, especially in an incorrect manner.
- Lumbar Spinal Stenosis- This condition arises when the nerves within the spinal canal are compressed. This then causes tissue to press against the nerves. Herniation, instability, degeneration, and a small spinal canal since birth are all common reasons for spinal stenosis to develop. Adults over 55 are the most common victims of spinal stenosis.
- Spinal Instability- As discs degenerate, the cushioning between the vertebrae decreases. This means that the bones are more likely to clash with one another. In turn, this leads to a more unstable spine. An orthopedic surgeon can restore the spine to its former functional state, improving overall body maneuverability.
- Vertebral Compression Fractures- Osteoporosis and other bone-softening conditions can cause the vertebrae to collapse. When this occurs, it can possibly lead to a fracture. Traumatic injuries like falls or car accidents can also lead to a compression fracture.
While these conditions are the most common ones that are treated by minimally invasive spine surgery, there are other less specific instances where it is used as well. For example, back-related injuries such as scoliosis, natural deformities, tumors and infections can all be treated with a minimally invasive surgery.

Want more information?
Contact the orthopedic professionals at Central Orthopedic to make an appointment today. Visit our offices in:
- Plainview
- Rockville Centre
7 Potential Complications of Spine Surgery
Complications are less common during minimally invasive procedures than open surgeries. These are some of the most common complications that occur as a result of minimally invasive spine surgery.
Discuss Your Options
Spinal surgery should not be taken lightly. Carefully discuss your options with your surgeon and understand potential risks and complications
- Infections- To prevent infections, orthopedic surgeons prescribe antibiotics to patients, both before and after the surgery. This greatly decreases the chance for an infection.
- Severe bleeding- As with any other surgery, some bleeding is anticipated after a spine surgery. Severe bleeding, however, is an indicator that something has gone wrong.
- Grafting location pain- While it is uncommon, some patients consistently experience pain located at the grafting site.
- Resurgence of pain- In some situations, the surgery might be unsuccessful. It’s possible for the original symptoms to return in cases like these.
- Pseudarthrosis- Most common for smokers, pseudarthrosis is a condition in which the bone does not fully form following a graft. To solidify the bone, a second surgery may be necessary.
- Nerve damage- Despite the extremely calculated and deliberate maneuvering of the orthopedic surgeon during this operation, nerve damage is unfortunately a possibility. This is exceptionally rare.
- Blood clots- During this procedure, it’s possible for blood to travel through the legs and into the lungs. This is not a common complication.
3 Spinal Surgery Recovery Challenges
Because the spinal muscle and tissue is not directly impacted during a minimally invasive procedure, there are less obstacles on the road to recovery for a minimally invasive procedure than an open surgery.
- Rest Period- Patients who undergo a minimally invasive surgery generally remain in the hospital for 2-3 days. This is in contrast to open spine surgery patients, who generally exit the hospital after 3-6 days.
- Physical Therapy- As each patient’s body reacts differently to surgery, the need for physical therapy varies. After the procedure, your orthopedic surgeon will confer with a physical therapist to outline a routine that will restore your full range of motion.
- Keep the Spine Aligned- During recovery, it’s important for patients to keep the spine aligned, thus ensuring that the spine will remain intact.

No Two Patients are the Same
Each patient’s spine has seen different conditions, obstacles, and has developed a certain way. These conditions inevitably lead to a large differences in spinal health. For this reason, it’s imperative that doctors take these factors into account. Our orthopedic surgeons will carefully evaluate each individual’s spine before deciding on a course of action. Central Orthopedics’ qualified staff will use the safest and most effective surgical methods to ensure your continued health.
